Overview
In 2019, WEconnect Health partnered with a Medicaid plan in Pennsylvania to implement the WEconnect platform with a select cohort of members. The plan introduced WEconnect to five providers who then referred members to the WEconnect platform. The providers included: two large health systems with inpatient and outpatient departments, an outpatient FQHC, and a chain of outpatient Medication-Assisted Treatment (MAT) facilities. With 200 members using the WEconnect platform, the pilot began in Q1 of 2019 and continued through Q2 of 2020.
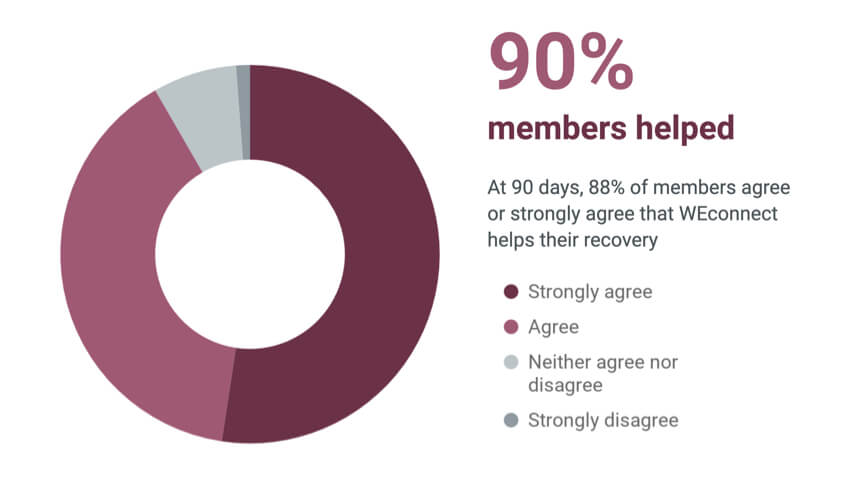
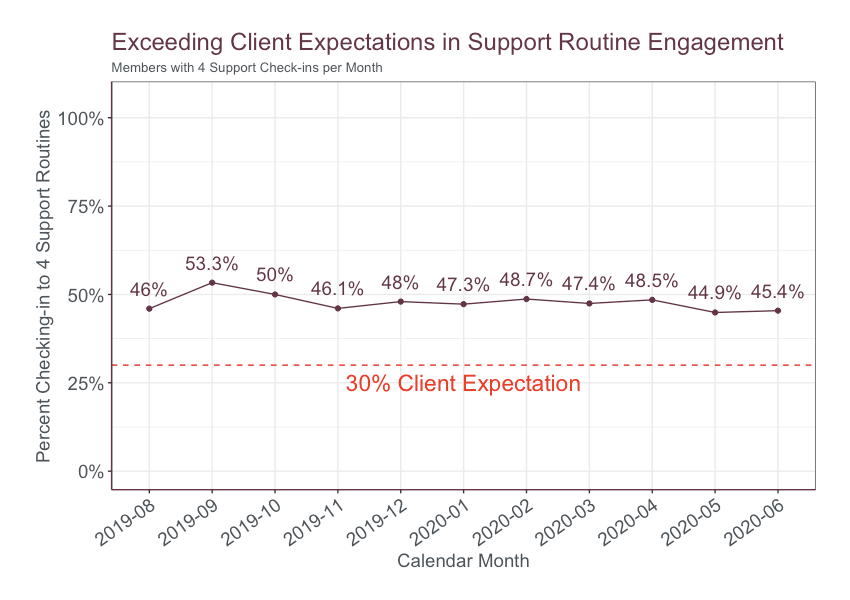
Prior to a long-term claims analysis, the program was evaluated based on a series of metrics assessing member engagement with their treatment plan. Targets were exceeded in almost all areas measured, including activation, engagement, retention, and helpfulness rate.

Claims Analysis
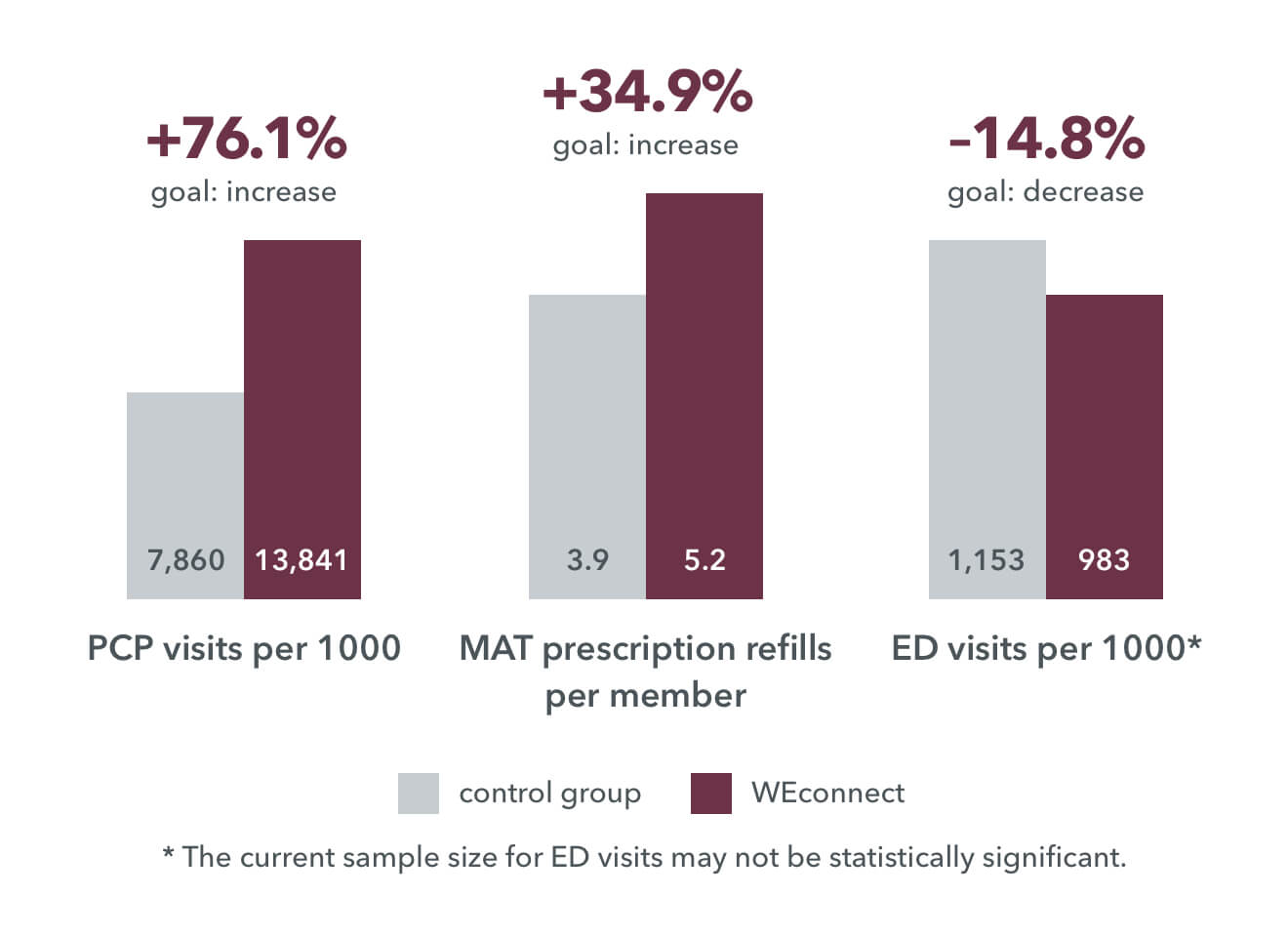
Of the 200 members on the WEconnect app, 95 were selected to be included in the claims analysis. Those 95 members were all patients at Crossroads treatment centers, and were chosen for comparison with the control group of Crossroads patients not using the WEconnect app. Controls were also matched on demographic data. The comparison resulted in the following:
The claims analysis showed a significant increase in PCP engagement and MAT refills among the WEconnect cohort. In the study, use of the WEconnect app was associated with a 76% higher rate of Primary Care Provider (PCP) engagement (p
Patients who engage with their PCP in an initial incentivized visit are more likely to develop a relationship with their doctor and continue to adhere to their treatment plans. Patients who see a PCP are also more likely to be referred to appropriate levels of outpatient care, and one study showed that this led to a decrease in non-emergent ED visits by 19% (p
Medication-Assisted Treatment (MAT, or pharmacotherapy), incentivized by use of the WEconnect app, is an extremely effective treatment for substance use disorder (SUD) that can significantly reduce long-term healthcare costs. Even including higher pharmacy expenses, studies show that a six-month period on MAT results in 29% lower overall annual health plan costs for members compared to those with no medication (Baser et al., 2011). In a 2010 five-year study, members on MAT had 50%–62% lower total annual commercial health plan costs (McCarty et al., 2010). Individuals who attended one or more MAT appointments had significantly fewer emergency room visits, recurrences of use (relapses), primary care visits, inpatient stays, and other non-addiction treatment visits.
References
- Baser, O., Chalk, M., Fiellin, D. A., & Gastfriend, D. R. (2011). Cost and utilization outcomes of opioid-dependence treatments. The American Journal of Managed Care, 17 Suppl 8, S235-248.
- Bradley, C., Neumark, D., & Walker, L. S. (2017). The Effect of Primary Care Visits on Health Care Utilization: Findings from a Randomized Controlled Trial (No. w24100; p. w24100). National Bureau of Economic Research. https://doi.org/10.3386/w24100
- McCarty, D., Perrin, N. A., Green, C. A., Polen, M. R., Leo, M. C., & Lynch, F. (2010). Methadone maintenance and the cost and utilization of health care among individuals dependent on opioids in a commercial health plan. Drug and Alcohol Dependence, 111(3), 235–240. https://doi.org/10.1016/j.drugalcdep.2010.04.018
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.
%202.svg)